Fatty Liver: The Definitive Guide (2024)
If you are searching for information on Fatty Liver – you have found the definitive guide. Fatty Liver is a common diagnosis by doctors and a cause of concern for millions of people throughout the world. After reading our guide, you will have all the information needed to tackle this important medical problem head-on.
Below you will also find 9 helpful suggestions that you can start immediately to reverse fatty liver.
Fatty Liver
It is normal for your liver to contain some fat. However, if more than 5% to 10% of your liver’s total weight is fat, then it is called Fatty Liver (Hepatic Steatosis). If this fat is accompanied with excess alcohol consumption, then it is the first stage of Alcoholic Liver Disease (ALD). If not, then it is the first stage of Nonalcoholic Fatty Liver Disease (NAFLD).
According to Harvard Medical School, up to 20% of American adults have some degree of fatty liver disease. A condition that used to occur primarily in people who drank excessively, the numbers have risen drastically in recent years due to the increase in obesity and diabetes. It affects between 70% and 90% of people with those conditions, so as obesity and diabetes have become more common, so has fatty liver disease.
What Is Nonalcoholic Fatty Liver Disease (NAFLD)?
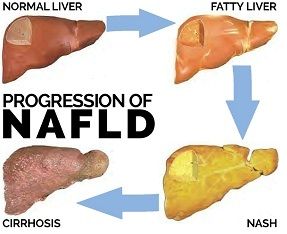
Nonalcoholic Fatty Liver Disease (NAFLD) is named for a grouping of liver abnormalities/diseases that progresses from the relatively harmless Fatty Liver, not due to excess alcohol consumption, to Nonalcoholic Steatohepatitis (NASH) to Cirrhosis.
NASH affects 2% – 5% of Americans and is diagnosed when a fatty liver is accompanied by varying degrees of inflammation and scarring of liver tissue and cells (fibrosis). Unlike Fatty Liver, NASH is not considered relatively harmless. Instead, NASH is considered a liver disease with the potential to progress to cirrhosis, which can then lead to liver failure.
Symptoms
Most people with fatty liver have no symptoms. When symptoms do occur, they may include:
- fatigue
- weight loss
- nausea
- abdominal pain
- spider-like blood vessels
- jaundice
- itching
- swelling in legs and feet
As you can see from the list above, when symptoms do occur, they don’t appear to directly be attributed to a liver problem. Fatigue and weakness are two examples of these such symptoms. However, sometimes the relationship is obvious. When a patient complains of pain or discomfort over the area of the liver, it could be caused by the stretching of the liver covering due to the increase in fat deposits and inflammation. The pain is usually dull and aching, not intense, sudden or severe. There is also no predictable pattern when the pain occurs.
While children can get fatty liver, it is a condition that usually manifests during middle age as a result of years of stress on the body. Diagnosis of NAFLD requires a blood test, imaging or biopsy of the liver.
Is it Reversible?
 The good news is that it is a reversible condition. With a few healthy lifestyle changes such as losing weight through proper diet and exercise, limiting over-the-counter (OTC) medications so fewer toxins enter the body, and avoiding alcohol and high-fat or high-sugared foods, Fatty Liver can be reversed in anywhere from three to six months to two years, depending on severity and adherence to a proper diet.
The good news is that it is a reversible condition. With a few healthy lifestyle changes such as losing weight through proper diet and exercise, limiting over-the-counter (OTC) medications so fewer toxins enter the body, and avoiding alcohol and high-fat or high-sugared foods, Fatty Liver can be reversed in anywhere from three to six months to two years, depending on severity and adherence to a proper diet.When left unchecked, however, it can lead to NASH, a much more serious condition. Those with NASH typically have inflammation and liver damage and the beginnings of scarring of the liver called fibrosis, which left unchecked can lead to cirrhosis of the liver.

Two Liver Functions That Directly Impact the Formation of Fat in the Liver
 There are two functions of the liver that directly impact the formation of excess fat in the liver: metabolism of carbohydrates (sugars) and digestion of lipids (fats). When we consume carbohydrates, our blood sugar rises triggering a rise in insulin. That rise in insulin signals our liver to begin storing the excess glucose within its own cells.
There are two functions of the liver that directly impact the formation of excess fat in the liver: metabolism of carbohydrates (sugars) and digestion of lipids (fats). When we consume carbohydrates, our blood sugar rises triggering a rise in insulin. That rise in insulin signals our liver to begin storing the excess glucose within its own cells.
When the liver is full, it begins storing the excess carbohydrates as fat in our body fat. Sometimes that fat begins to accumulate in the liver cells, and the liver becomes fat.
Similarly, when we consume more lipids that the body can use for energy, the liver stores the excess lipids in body fat, and this excess of lipids can begin to accumulate within the liver as well. Whether the excess of food is made up of carbohydrates (sugars) or fat (lipids) – the liver stores the excess energy for future use. Often this will result in excess fat accumulating in the liver itself. This is known as Fatty Liver, the first stage of NAFLD and should be viewed as a warning to change unhealthy lifestyle habits and adopt a low carbohydrate and low fat diet that is high in fresh vegetables and lean proteins.
Causes
One of the primary functions of the liver is the metabolism of fat. Several factors can interfere with this process, including certain diseases, poor diet, certain medications and exposure to toxic substances.

Fatty Liver can also be the result of several conditions and diseases, such as:
- Diabetes (Type 2)
- Being overweight or obese
- High cholesterol or triglycerides
- Metabolic syndrome
- Polycystic ovary syndrome
- Sleep apnea
- Underactive thyroid (hypothyroidism)
- Underactive pituitary gland (hypopituitarism)
Because Nonalcoholic Fatty Liver Disease has been linked to insulin resistance, the two most common causes of this condition are obesity and diabetes (Type 2). A fatty liver is typically found in those who carry excess weight around the midsection.
Diagnosis
During an exam a doctor may detect an enlarged liver and signs of cirrhosis like ascites (fluid buildup in the abdominal cavity). An enlarged spleen might also be present but only in people with NASH. There is no single test that can accurately diagnose fatty liver or NASH. A diagnosis of NASH is made only after all other causes of fatty liver and causes of elevated liver enzymes have been excluded.
Blood work can be done to test for any abnormalities. Typically elevations in liver enzymes – whereby the level of ALT elevation is higher than the level of AST – elevation could be an indicator of fatty liver or NASH.
 Ultrasounds can also be used for diagnosis. However, an ultrasound needs a skilled operator. In addition, the sensitivity of the scan is decreased in people with high amounts of abdominal fat. A CT (computerized tomography) scan could be performed as well and may even measure the degree of fat in the liver, but this determination can be hampered if there are any liver iron deposits. Imaging studies can detect the presence of fat in the liver but not the severity.
Ultrasounds can also be used for diagnosis. However, an ultrasound needs a skilled operator. In addition, the sensitivity of the scan is decreased in people with high amounts of abdominal fat. A CT (computerized tomography) scan could be performed as well and may even measure the degree of fat in the liver, but this determination can be hampered if there are any liver iron deposits. Imaging studies can detect the presence of fat in the liver but not the severity.Therefore, one can presume a diagnosis of fatty liver or NASH based on signs of insulin resistance, elevated ALT levels for a long duration, signs of fatty liver through imaging and exclusion of other causes of elevated ALT levels and fatty liver.
Only a liver biopsy can definitively diagnose a fatty liver and NASH as well as the amount of fatty deposits, degree of inflammation and extent of damage to the liver.
Treatment
Treatment involves first taking corrective action to reduce excess sugar and fat from the diet, losing weight and maintaining a healthy weight while getting regular exercise. If there is damage to the liver such as inflammation or scarring, your physician may prescribe medications. It is important to take action to manage NAFLD before the conditions progresses to the next stage of liver disease, Nonalcoholic Steatohepatitis (NASH), as this can lead to cirrhosis.
9 Helpful Suggestions for Reversing Fatty Liver, NAFLD and NASH
- Diet – The liver cannot detect carbohydrates (sugar) in the blood so it relies on the corresponding rise in insulin to trigger the processing of excess sugar into fat. A diet that is high in lipids (fat) and carbohydrates overloads the liver and fat begins to accumulate in the organ itself. To correct this, a diet low in sugars and fat is essential. In addition, a diet high in fiber has been shown to reduce blood cholesterol levels by up to 10%. A healthy diet that limits not only calorie consumption but also limits carbohydrates and saturated fats to about 10% of total calories will aid in losing excess weight and maintaining a healthy weight. Keep in mind that weight loss must be achieved slowly through a doctor’s recommended plan of diet and exercise. Weight loss should not be accomplished through quick or fad dieting, as this can actually exacerbate disease progression. Also, weight loss must be maintained or the disease may come back.
- Exercise – At the basic level, exercise burns calories (energy) from both carbohydrates and fats, taking some of the excess out of the blood and, over time, out of stored fat. Exercise also helps increase insulin sensitivity, allowing cells to take up glucose more effectively during and after exertion. Through its decrease of glucose both in the blood and liver, exercise reduces the load on the liver and helps decrease the accumulation of fat in the organ itself.
- Diabetes Control – Working with your physician to manage diet, exercise and medications necessary to maintain steady blood glucose is vital to managing diabetes. Up to 70% of those with NAFLD and NASH have Type 2 diabetes or are obese, so maintaining a healthy weight and managing symptoms of diabetes is a key element of reversing NAFLD.
- Cholesterol Control – For many, simply managing intake of fats is not enough. The use of statins has been shown to show some improvement in patients with NAFLD, and more research is ongoing.
- Avoid Toxic Chemicals – Over 10,000 household and personal products contain chemicals that are potentially dangerous. To avoid harmful chemicals, eat real, unprocessed foods, choose organic and non-GMO foods, store food in glass containers rather than plastic, replace non-stick pots and pans with ceramic, use a vacuum with a HEPA filter, avoid products with fragrances and harsh commercial cleaning chemicals.
- Avoid Over-the-Counter Medications – One of the liver’s primary functions is to filter toxic chemicals from the blood. Many over-the-counter medications include chemicals that must be filtered out of the body, increasing stress on the liver.
- Antioxidants – A diet rich in foods that offer antioxidants such as vitamins C and E offer protection and reduce inflammation and oxidative stress on liver cells, minimizing potential damage from lesions and scarring. Foods containing antioxidants include green tea, fruits and vegetables, garlic, and certain spices such as turmeric.
- Milk Thistle – Is the #1 herb recommended to support and protect the liver. Studies have shown that silymarin, the active ingredient in milk thistle, is effective in reducing inflammation and steatosis in liver cells and regenerating new, healthy liver cells. Silymarin has also been shown to provide antioxidant protection and have anti-fibrotic properties.
- Medications – Medications such as Metformin and lipid-reducing statins may be prescribed by your physician.
Fatty Liver Diet
When diagnosed by a doctor or medical professional – one of the first recommendations is that the patient changes his or her diet.
What not to eat when you have a fatty liver:
- Alcohol
- Sugar
- Soda
- Artificial trans fat
- High glycemic carbohydrates
Moreover, Eat more ‘real’ food with substance and nutritional value.
The kind of foods you should eat:
- Whole grains
- Healthy fats
- Protein at every meal
- Plenty of produce
To learn more about Fatty Liver Diet and the many benefits of healthy eating when trying to reverse Fatty Liver – please see our Fatty Liver Diet page.
This information is intended for educational purposes only and should not be used in any other manner. This information is not intended to substitute for informed medical advice. You should not use this information to diagnose or treat a health problem or disease without consulting with a qualified health care provider.
Suggested Articles:
- FDA Grants Fast Track Designation for NAFLD and NASH Combination Therapy
- Overeating Will Be The Main Reason for Liver Transplants in 5 Years
- Diagnosing and Managing Nonalcoholic Fatty Liver Disease (NAFLD)
- Green Tea Promotes a Lean Liver
- Psychological Tool to Reverse Fatty Liver Disease
- Newly Revealed Health Risk Linked to Fatty Liver Disease
- How to Prevent a Fatty Liver
American Heart Association. (2016). Good vs. bad cholesterol. American Heart Association. Retrieved on 3/29/16 from http://www.heart.org/HEARTORG/Conditions/Cholesterol/AboutCholesterol/Good-vs-Bad-Cholesterol_UCM_305561_Article.jsp#.VvrbHUenwaE.
Cabot, S., MD.; Eanelli, T., MD. (2010). Fatty liver: You can reverse it. Glendale, AZ: S.C.B. Inc. International.
Cacciapuoti, F.; Scognamilglio, A.; Palumbo, R.; Forte, R.; Cacciapuoti, F. (2013). Silymarin in nonalcoholic fatty liver disease. World Journal of Hematology. 5(3): 109–113. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3612568/pdf/WJH-5-109.pdf.
Diabetes Association. (2016). Blood glucose control and exercise. Diabetes.org. Retrieved on 3/29/16 from http://www.diabetes.org/food-and-fitness/fitness/get-started-safely/blood-glucose-control-and-exercise.html.
Egan, M.; Prasad, S. (2011). Statins for patients with nonalcoholic fatty liver? The Journal of Family Practice. 60(9): 536–538. Retrieved on 3/29/16 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3183966/pdf/JFP-60-536.pdf.
FDA. (2015). FDA revises proposed Nutrition Facts label rule to include a daily value for added sugars. Food and Drug Administration. Retrieved on 3/29/16 from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm455837.htm.
Gebel, E. (2012). The liver’s role: How it processes fats and carbs. Diabetes Forecast. Retrieved on 3/28/16 from http://www.diabetesforecast.org/2012/feb/the-liver-s-role-how-it-processes-fats-and-carbs.html?print=t.
Harvard Health Publications. "When the liver gets fatty." Retrieved on 4/20/16 from http://www.health.harvard.edu/diseases-and-conditions/when-the-liver-gets-fatty
Healthline. (2015). Fatty liver. Healthline.com. Retrieved on 3/28/16 from http://www.healthline.com/health/fatty-liver#Overview1.
Healthline. (2016). Fatty liver: Who’s at risk for fatty liver? Healthline.com. Retrieved on 3/28/16 from http://www.healthline.com/health/fatty-liver#RiskFactors5.
Herrine, S.K., MD. (2016). Fatty liver (Steatosis). MerckManuals.com. Retrieved on 3/28/16 from https://www.merckmanuals.com/home/liver-and-gallbladder-disorders/manifestations-of-liver-disease/fatty-liver.
Herrine, S.K., MD. (2016). Nonalcoholic Steatohepatitis (NASH). MerckManuals.com. Retrieved on 3/28/16 from https://www.merckmanuals.com/professional/hepatic-and-biliary-disorders/approach-to-the-patient-with-liver-disease/nonalcoholic-steatohepatitis-nash.
Herrine, S.K., MD. (2016). Liver structure and function. MerckManuals.com. Retrieved on 3/28/16 from https://www.merckmanuals.com/professional/hepatic-and-biliary-disorders/approach-to-the-patient-with-liver-disease/liver-structure-and-function.
John Hopkins Editors. (2016). Nonalcoholic fatty liver disease. John Hopkins Medicine. Retrieved on 3/31/16 from http://www.hopkinsmedicine.org/healthlibrary/conditions/liver_biliary_and_pancreatic_disorders/nonalchololic_fatty_liver_disease_134,178/.
Mayo Clinic Editors. (2016). Dietary fats: Which type to choose. Mayo Clinic.org. Retrieved on 3/31/16 from http://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fat/art-20045550.
Medline Plus. (2016). Carbohydrates. U.S. Library of Medicine. Retrieved on 3/31/16 from https://www.nlm.nih.gov/medlineplus/carbohydrates.html.
Medline Plus. (2016). Protein in diet. U.S. National Library of Medicine. Retrieved on 3/31/16 from https://www.nlm.nih.gov/medlineplus/ency/article/002467.htm.
Mercola, Dr. (2015). Toxic chemical health risks. Mercola.com. Retrieved on 3/29/16 from http://articles.mercola.com/sites/articles/archive/2015/12/08/toxic-chemical-health-risks.aspx.
NIH. (2012). How does the liver work? PubMed Health. Retrieved on 3/28/16 from http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072577/.
NIH. (2016). Nonalcoholic steatohepatitis. National Institute of Diabetes and Digestive and Kidney Disease. Retrieved on 3/31/16 http://www.niddk.nih.gov/health-information/health-topics/liver-disease/nonalcoholic-steatohepatitis/Pages/facts.aspx.
NIH. (2016). What is cholesterol? National Heart, Lung and Blood Institute. Retrieved on 3/29/16 from http://www.nhlbi.nih.gov/health/health-topics/topics/hbc.
Pais, P. D’Amato, M. (2014). In vivo efficacy study of milk thistle extract (ETHIS-094â„¢) in STAMâ„¢ model of nonalcoholic steatohepatitis. Drugs in R&D. 14(4): 291-299. Retrieved on 3/30/16 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4269824/pdf/40268_2014_Article_68.pdf.
Penner, E. (2015). Ask the dietitian: What’s the best carb, protein, and fat breakdown for weight loss? My Fitness Pal: Ask the Dietitian. Retrieved on 3/31/16 from http://blog.myfitnesspal.com/ask-the-dietitian-whats-the-best-carb-protein-and-fat-breakdown-for-weight-loss/.
Tolman, K.G.; Dalpiaz, A.S. (2007). Treatment of nonalcoholic fatty liver disease. Therapeutics and Clinical Risk Management. 3(6): 1153-1163. Retrieved on 3/29/16 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2387293/pdf/tcrm-0306-1153.pdf.
USDA. (2016). HHS and USDA Release New Dietary Guidelines to Encourage Healthy Eating Patterns to Prevent Chronic Diseases. United States Department of Agriculture. Retrieved on 3/29/16 from http://www.fns.usda.gov/pressrelease/2016/000516.
Web MD. (2016). Digestive disorders. WebMD.com. Retrieved on 3/28/16 from http://www.webmd.com/digestive-disorders/picture-of-the-liver.
Zeratsky, K. (2016). Nutrition and healthy eating. Mayo Clinic.org. Retrieved on 3/31/16 from http://www.mayoclinic.org/fat-grams/expert-answers/FAQ-20058496?p=1.